The intricate dance of drug absorption within the human body is a marvel of biological engineering, but it also presents a significant challenge for medical professionals and patients alike. A groundbreaking study by researchers at MIT, Brigham and Women’s Hospital, and Duke University has brought us closer to ensuring that the drugs we take are not only effective but safe when taken in combination with others.
At the heart of this issue is the fact that orally administered drugs must navigate the complex environment of the digestive tract, relying on transporter proteins to enter the bloodstream. Until now, the specific transporters that drugs use have been somewhat of a mystery, leading to potential adverse interactions when multiple drugs compete for the same transport pathway.
The recent study, led by Giovanni Traverso and his team, has developed a multipronged strategy to demystify this process. By combining tissue models with machine-learning algorithms, they have successfully identified which transporters are used by various drugs. This innovative approach has already made a significant discovery: a commonly prescribed antibiotic and a blood thinner can interfere with each other, a finding that could have profound implications for patient care.
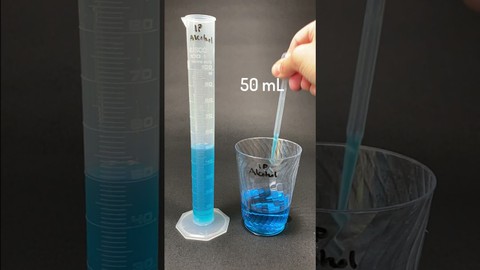
The methodology is as ingenious as it is effective. Researchers adapted a tissue model based on pig intestinal tissue to measure drug absorbability. By knocking down the expression of each transporter in the tissue, they could determine the specific pathways drugs take. This data, along with information from several drug databases, was then used to train a machine-learning model. The model’s ability to predict drug interactions is based on the chemical structure of the drugs, a testament to the power of artificial intelligence in healthcare.

The practical applications of this research are vast. The machine-learning model analyzed a new set of 28 currently used drugs and 1,595 experimental drugs, yielding nearly 2 million predictions of potential drug interactions. Among these was the interaction between doxycycline and warfarin, a blood thinner, which was confirmed by patient data. This interaction had previously gone undetected, highlighting the model’s potential to uncover hidden risks in drug prescriptions.
Moreover, this approach is not just about identifying risks; it’s also about enhancing the development of new drugs. Drug developers can now use this technology to fine-tune the formulation of new drug molecules, improving their absorbability and reducing the likelihood of interactions. The biotech company Vivtex is already pursuing this avenue, aiming to develop new oral drug delivery systems that are both safe and effective.
The deal with patient treatment is pretty straightforward. With this model, healthcare providers can make better decisions about giving out drugs, which could lower the chances of bad reactions that mess up treatments or even cause toxicity. Looking ahead, this research could be the start of a whole new way of doing medicine, where treatments are customized not just for the disease but for the person’s own biology.The research, generously funded by the National Institutes of Health and other prestigious institutions, highlights the importance of collaboration in advancing the boundaries of medical science. It serves as a wonderful illustration of how combining diverse expertise can spark innovative ideas in the field of healthcare.
The development of this machine-learning model is a significant step forward in the quest to make drug use safer for everyone. As we continue to unravel the complexities of drug interactions, we can look forward to a future where personalized treatment plans minimize risks and maximize the efficacy of the medications we rely on to maintain our health.
Related posts:
New model identifies drugs that shouldn’t be taken together
learning algorithm indentifies drugs that shouldn’t be prescribed together
New machine-learning model identifies drug interactions for safer prescribing